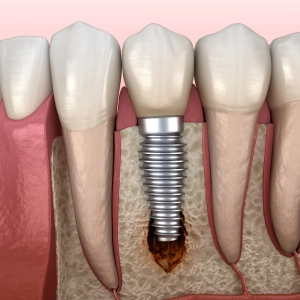
Dental implants are a popular and effective solution for replacing missing teeth. However, concerns have been raised about whether dental implants can lead to bone loss. The short answer is no, dental implants themselves do not cause bone loss. In fact, they can even help preserve the jawbone by providing stimulation similar to that of natural tooth roots. However, complications such as peri-implantitis, inadequate osseointegration, and poor oral hygiene can contribute to bone loss around dental implants, leading to potential implant failure and other issues.
Why Does Bone Loss Occur Around A Dental Implant
Several factors can contribute to bone loss around dental implants. These include peri-implantitis, inadequate osseointegration,trauma or injury, and poor oral hygiene. Additionally, systemic conditions such as osteoporosis and diabetes can also impact bone health and contribute to bone loss around dental implants.
Peri-implantitis:
Peri-implantitis is inflammation and infection around dental implants, similar to gum disease around natural teeth. It’s caused by bacteria, leading to gum inflammation and bone loss. Symptoms include redness, swelling, bleeding gums, and implant loosening. Risk factors include poor oral hygiene, smoking, diabetes, and immune issues. Prevention involves good oral care, regular check-ups, quitting smoking, and managing health conditions. Treatment includes professional cleaning, antimicrobial therapy, and surgery if severe. Early intervention is crucial to prevent implant loss.
Inadequate Osseointegration:
Inadequate osseointegration refers to insufficient bonding between the dental implant and the surrounding bone. This can result from various factors, including poor bone quality, improper implant placement, or inadequate healing time. Signs include implant mobility, discomfort, or pain. Factors affecting osseointegration include patient health, smoking, and bone quality. Preventive measures include proper implant placement, ensuring good bone quality, and following postoperative care instructions. Treatment may involve bone grafting or implant replacement to promote better integration. Regular follow-ups with the dentist are essential to monitor osseointegration progress and address any issues promptly.
Trauma or Injury:
Trauma or injury to the area around a dental implant can lead to bone loss. Accidents, sports injuries, or surgical complications can cause trauma, disrupting the healing process and affecting the stability of the implant. Signs of trauma-related bone loss include pain, swelling, or implant mobility. Preventive measures include wearing mouthguards during physical activities, following postoperative care instructions, and seeking immediate dental attention in cases of trauma. Treatment may involve stabilizing the implant, addressing any soft tissue damage, and promoting proper healing to prevent further bone loss. Regular dental check-ups can help detect and address any issues early on to minimize bone loss and preserve implant stability.
Poor Oral Hygiene:
Neglecting proper oral hygiene can contribute to bone loss around dental implants. Plaque and bacteria accumulation on the implant surface can lead to inflammation of the surrounding gum tissues, a condition known as peri-implantitis. Over time, untreated peri-implantitis can cause bone loss and compromise the stability of the implant. Maintaining good oral hygiene practices such as brushing twice daily with a soft-bristled toothbrush, flossing between implants and natural teeth, and using antimicrobial mouthwash can help prevent plaque buildup and reduce the risk of peri-implantitis. Regular dental visits for professional cleanings and exams are also essential for monitoring implant health and addressing any early signs of peri-implantitis promptly.
Systemic Health Conditions:
Certain systemic health conditions, such as diabetes, osteoporosis, and autoimmune disorders, can increase the risk of bone loss around dental implants. Diabetes, for example, can impair the body’s ability to heal and fight infection, making individuals with diabetes more susceptible to complications after implant placement. Similarly, osteoporosis can weaken the bones, including the jawbone, compromising the stability of dental implants. Autoimmune disorders like rheumatoid arthritis may also affect bone health and contribute to implant failure. Patients with these systemic health conditions should work closely with their healthcare providers to manage their conditions effectively and minimize the risk of complications related to dental implants. Additionally, a thorough medical evaluation and consultation with a dental implant specialist are crucial to assessing the suitability of implant treatment and developing a personalized treatment plan that considers the patient’s overall health status.
Smoking:
Smoking is a significant risk factor for bone loss around dental implants. The chemicals present in tobacco smoke can interfere with the body’s ability to heal and repair tissues, including the bone surrounding implants. Smoking restricts blood flow to the gums and bones, leading to decreased oxygen and nutrient delivery to the implant site, which impairs healing and increases the likelihood of implant failure. Moreover, smoking weakens the immune system, making smokers more susceptible to infections, such as peri-implantitis, which further accelerates bone loss. Patients who smoke are advised to quit or reduce smoking before undergoing dental implant surgery to improve the success rate and long-term stability of implants. Additionally, quitting smoking after implant placement can help mitigate the risk of complications and enhance the overall health of the gums and supporting bones.
Can it be Prevented?
Although total prevention of bone loss surrounding dental implants may not always be feasible, there are a number of strategies that can greatly lower the risk and decelerate the rate of bone loss. Here are a few methods of prevention:
- Maintain good oral hygiene practices, including brushing and flossing regularly.
- Attend regular dental check-ups and cleanings to monitor the health of your implants.
- Avoid smoking, as it can increase the risk of complications such as peri-implantitis.
- Follow any post-operative instructions provided by your dentist or oral surgeon.
- Manage systemic health conditions such as diabetes effectively to reduce the risk of complications.

What Can Be Done For The Bone Loss ?
Treatment Options for Bone Loss Around a Dental Implant:
Non-Surgical Intervention:
Professional Cleaning:
Thorough cleaning of the implant surface and surrounding tissues to remove plaque and calculus buildup.
Antimicrobial Therapy:
Prescription of antimicrobial agents or mouth rinses to control bacterial infection and inflammation.
Local Delivery of Antibiotics:
Application of antibiotic gels or solutions directly into the peri-implant pocket to target microbial pathogens.
Surgical Procedures:
Open Flap Debridement:
Surgical access to the implant site to remove infected or inflamed tissue and promote healing.
Bone Grafting:
Augmentation of bone volume using autogenous, allogenic, or synthetic bone graft materials to restore lost bone support.
Guided Bone Regeneration (GBR):
Placement of barrier membranes to protect bone grafts and facilitate new bone formation in defect areas.
Bone Regeneration Techniques:
Utilization of growth factors or bone-stimulating agents to enhance bone healing and regeneration around the implant.
Implant Surface Modification:
Surface Decontamination:
Mechanical or chemical treatment of the implant surface to remove biofilm and promote tissue integration.
Surface Coatings:
Application of bioactive coatings or modifications to enhance osseointegration and reduce bacterial adhesion.
Corrective Measures:
Implant Repositioning:
Adjustment of implant position or angulation to alleviate stress on the surrounding bone and optimize biomechanical support.
Prosthetic Modifications:
Evaluation and adjustment of prosthetic components to distribute occlusal forces evenly and prevent overloading.
Maintenance and Follow-Up:
Regular Monitoring:
Scheduled follow-up visits with the dental provider to assess implant stability, peri-implant tissue health, and bone level changes.
Professional Maintenance:
Routine maintenance procedures such as professional cleanings, periodontal therapy, and occlusal adjustments are necessary to prevent recurrence of bone loss.
Patient Education:
Education on proper oral hygiene practices, lifestyle modifications, and adherence to recommended treatment protocols will support long-term implant success.
If I am Diabetic, Will it Matter?
If you are diabetic, it can significantly impact your dental health and the success of dental implant procedures. Diabetes can affect your body’s ability to heal properly, increasing the risk of complications after implant surgery. Poorly managed diabetes may lead to slower healing, a higher susceptibility to infections, and a higher chance of implant failure. Additionally, diabetes can contribute to bone loss, which is crucial for the stability of dental implants. Therefore, it is essential to work closely with your dentist and healthcare provider to manage your diabetes effectively before undergoing any dental implant procedures. They can provide personalized recommendations and closely monitor your oral health to minimize risks and ensure successful treatment outcomes.
Conclusion
While dental implants themselves do not cause bone loss, various factors can contribute to bone loss around implants, leading to potential complications. However, with proper oral hygiene, regular dental care, and appropriate treatment interventions, the risk of bone loss can be minimized, allowing individuals to enjoy the benefits of dental implants for years to come. If you’re considering dental implants or have concerns about bone loss, schedule a consultation with your dentist to discuss your options and ensure optimal oral health. Visit Smile Boutique to learn more and schedule your appointment today.




